GAO Highlights VA EHR Problems
Per the notice below, the United States Government Accountability Office (GAO) is highlighting the many problems the Veterans Administration (VA) is having implementing a new electronic health record (EHR) system.
Veterans Affairs’ Ongoing Struggle to Modernize Its Electronic Health Record System
After three unsuccessful attempts, the Department of Veterans Affairs is currently on its fourth effort to modernize its outdated electronic health records system. VA relies on its electronic health record system to manage the health care needs of nearly 9 million veterans and their families. But the department’s latest attempt to modernize this system is also delayed and faces similar issues seen in prior efforts. Today’s WatchBlog post looks at our new report on the status of VA’s efforts and its challenges. GAO’s Carol Harris also testified before Congress about this issue in February. Learn more in the video below.
What’s going on with VA’s electronic health records rollout?
The current electronic health record system used by the VA is more than 30 years old, complex, and costly to maintain. VA’s efforts to replace its aging legacy system began in 2001. Its first three attempts were abandoned due to concerns about project planning, high costs, and undelivered capabilities. VA’s fourth attempt began in 2018 and a new system was deployed to six medical centers at a cost of about $12.7 billion. The rollout was paused in April 2023, after users reported concerns including patient safety and system reliability issues. Many of these users are medical professionals and administrators who need the system to support providing health care to veterans.
An emergency room nurse reviews the patient status board
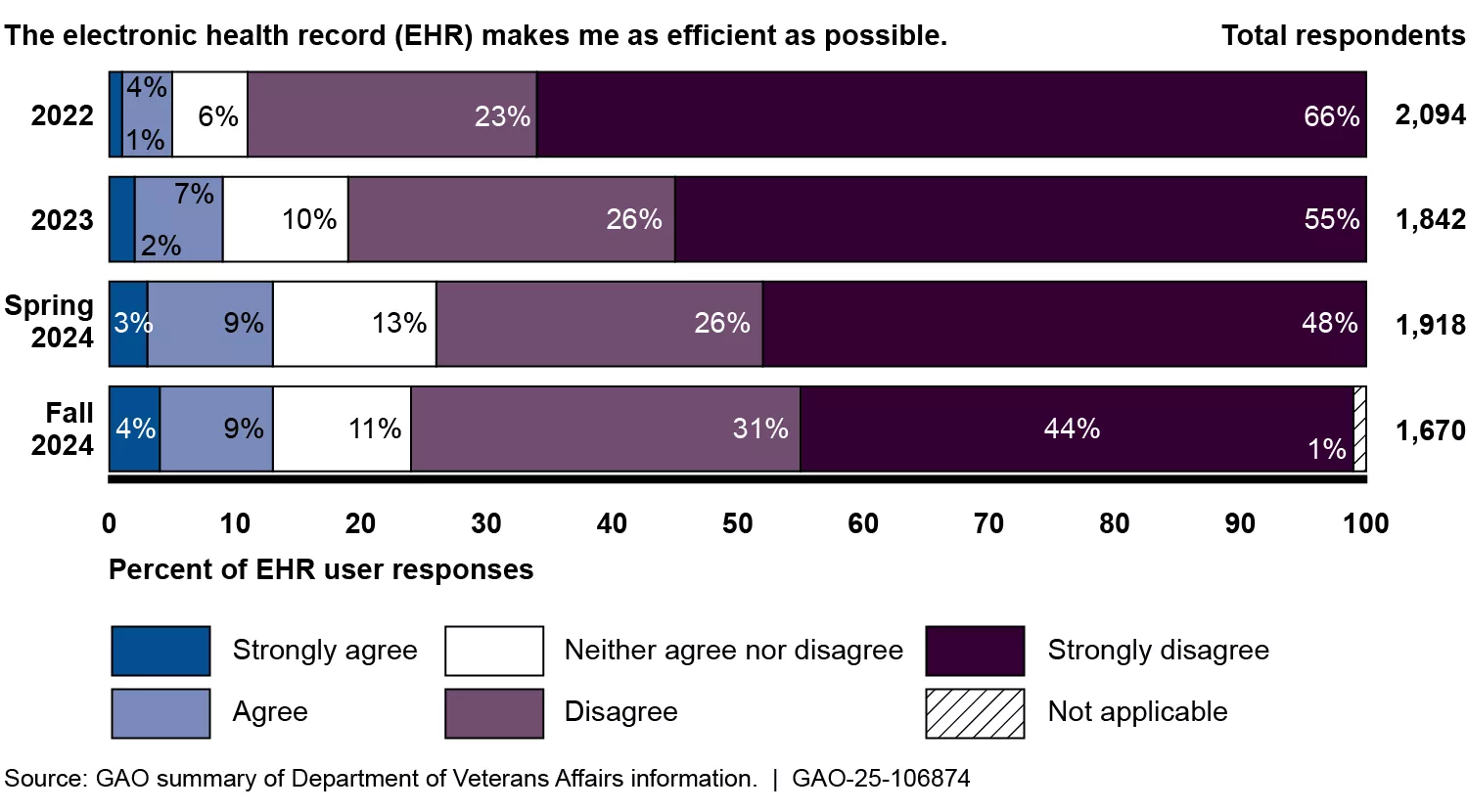
We have issued several reports about VA’s modernization efforts throughout the years. One concern highlighted in our earlier work was that the department did not have adequate measures for assessing the extent to which users' needs were addressed. Since then, user feedback has improved slightly. But in 2024, 75% of users disagreed that the modernized system made them as efficient as possible.
What’s next for VA?
Since pausing the rollout of its fourth attempt, VA has made incremental improvements to its new system. But much more needs to be done. For example, as of June 2024, VA had implemented more than 1,500 configuration changes to the system. But it still has not addressed about 1,800 additional changes that have been requested. VA also has not assessed the impacts of its pause of the new system's rollout on deployment schedule and cost. In 2019, the estimated 10-year cost of implementing and maintaining a new electronic health record system was about $16.1 billion. In 2022, an independent source estimated costs of $49.8 billion. However, these estimates do not reflect the full magnitude of changes to VA’s investment. Over the years, we’ve made 18 recommendations to improve VA’s efforts, including 3 new recommendations in our latest report. Of the older recommendations (15 of them), VA has implemented just one. The remaining 14 and our newest recommendations are critical to reducing risks involved with rolling out a new electronic health record system, as well as delivering a quality system that meets users’ needs. Learn more about this issue in our latest report.


